First about Locus Coeruleus
Locus coeruleus: a new look at the blue spot – PMC
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8991985/
”The locus coeruleus (LC), or ‘blue spot’, is a small nucleus located deep in the brainstem that provides the far-reaching noradrenergic neurotransmitter system of the brain. This phylogenetically conserved nucleus has proved relatively intractable to full characterization, despite more than 60 years of concerted efforts by investigators. Recently, an array of powerful new neuroscience tools have provided unprecedented access to this elusive nucleus, revealing new levels of organization and function. We are currently at the threshold of major discoveries regarding how this tiny brainstem structure exerts such varied and significant influences over brain function and behaviour. All LC neurons receive inputs related to autonomic arousal, but distinct subpopulations of those neurons can encode specific cognitive processes, presumably through more specific inputs from the forebrain areas. This ability, combined with specific patterns of innervation of target areas and heterogeneity in receptor distributions, suggests that activation of the LC has more specific influences on target networks than had initially been imagined.”
The role of the locus coeruleus in the generation of pathological anxiety – PM
BvS-< also function ”hormone-like in many processes
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7479871/
”This review aims to synthesise a large pre-clinical and clinical literature related to a hypothesised role of the locus coeruleus norepinephrine system in responses to acute and chronic threat, as well as the emergence of pathological anxiety. The locus coeruleus has widespread norepinephrine projections throughout the central nervous system, which act to globally modulate arousal states and adaptive behavior, crucially positioned to play a significant role in modulating both ascending visceral and descending cortical neurocognitive information. In response to threat or a stressor, the locus coeruleus–norepinephrine system globally modulates arousal, alerting and orienting functions and can have a powerful effect on the regulation of multiple memory systems. Chronic stress leads to amplification of locus coeruleus reactivity to subsequent stressors, which is coupled with the emergence of pathological anxiety-like behaviors in rodents. While direct in vivo evidence for locus coeruleus dysfunction in humans with pathological anxiety remains limited, recent advances in high-resolution 7-T magnetic resonance imaging and computational modeling approaches are starting to provide new insights into locus coeruleus characteristics.”
The Locus Coeruleus- Norepinephrine System in Stress and Arousal: Unraveling Historical, Current, and Future Perspectives – PMC
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7873441/
”Arousal may be understood on a spectrum, with excessive sleepiness, cognitive dysfunction, and inattention on one side, a wakeful state in the middle, and hypervigilance, panic, and psychosis on the other side. However, historically, the concepts of arousal and stress have been challenging to define as measurable experimental variables. Divergent efforts to study these subjects have given rise to several disciplines, including neurobiology, neuroendocrinology, and cognitive neuroscience. We discuss technological advancements that chronologically led to our current understanding of the arousal system, focusing on the multifaceted nucleus locus coeruleus. We share our contemporary perspective and the hypotheses of others in the context of our current technological capabilities and future developments that will be required to move forward in this area of research.”
Arousal: The word/concept arousal is often used without the user thinking about definition or not well defined – simply because our knowledge of the brain’s complex synergy interaction processes is limited.
The definition (based on my paradigm, see https://biopsychosocialmedicine.com/paradigm/) that I work with is ”dysfunctional dominances and/or increases in excitatory neurotransmitters, all categories and possibly even systems that are not considered neurotransmitter related” that can be temporary or chronic that vary between and within individuals over situation and time”.
Arousal is usually associated with sexual and stress arousal, where we focus on stress (sympathetic and brainstem related), and especially on the Locus Coeruleus, LC, and NE
”In summary, the LC-norepinephrine system is a pontine neuro modulatory nucleus with broad projections throughout the forebrain, cerebellum, and spinal cord. Classic studies have implicated LC in a myriad of functions such as arousal, behavioral flexibility, learning, memory, and wakefulness … LC activity is low during REM sleep, since muscle tone is lost (Szabadi, 2013; Sara, 2017)” BvS -> See below*. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7034292/
“Arousal may be understood on a spectrum, with excessive sleepiness, cognitive dysfunction, and inattention on one side, a wakeful state in the middle, and hypervigilance, panic, and psychosis on the other side. However, historically, the concepts of arousal and stress have been challenging to define as measurable experimental variables. Divergent efforts to study these subjects have given rise to several disciplines, including neurobiology, neuroendocrinology, and cognitive neuroscience. We discuss technological advancements that chronologically led to our current understanding of the arousal system, focusing on the multifaceted nucleus locus coeruleus. We share our contemporary perspective and the hypotheses of others in the context of our current technological capabilities and future developments that will be required to move forward in this area of research. … ater studies by Aston-Jones and Bloom not only confirmed but also more accurately described the involvement of LC-NE activity in RAS. Their findings demonstrated that LC tonic discharge rates were highest in the waking state, slower in SWS, and absent in REM sleep (110), thus firmly establishing a foundation for LC-NE involvement in the RAS that controls sleep-wake cycles.” https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2020.601519/full
But also specifically on chronic LC/NE (in e.g. PTSD, but NB it is very difficult to reasonably accurately follow its variations with current measurement methods) and even more specifically on LC/NE’s relationship to *REM sleep.
“Sleep is critical for proper memory consolidation. The locus coeruleus (LC) releases norepinephrine throughout the brain except when the LC falls silent throughout rapid eye movement (REM) sleep and prior to each sleep spindle during NREM sleep.” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7556718/
“During most stages of sleep, the thalamus becomes quiet, letting you tune out the external world. But during REM sleep, the thalamus is active, sending the cortex images, sounds, and other sensations that fill our dreams … “ https://www.ninds.nih.gov/health-information/public-education/brain-basics/brain-basics-understanding-sleep BvS-> but LC/NE inactive during REM-sleep, see above).
Wiring Diagram of the RAS (Reticular Activation Systems)
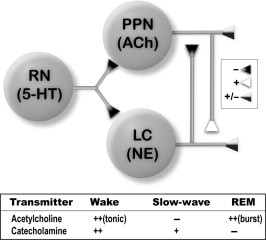
Figure 4.1. Wiring diagram of the RAS. Top. Recordings in slices have shown that the dorsal raphe nucleus (RN), mostly made up of serotonergic (5-HT) cells, generally inhibits (filled triangles) the pedunculopontine nucleus (PPN), which has cholinergic (ACh) cells among others, and the locus coeruleus (LC), which is made up mostly of noradrenergic (NE) cells. The LC inhibits the PPN, while the PPN excites LC neurons (open triangle). Both the PPN and LC project in parallel to ascending and descending sites and modulate these (half-filled triangles). Bottom. Table showing the overall firing patterns of these cell groups during different wake–sleep states. Cholinergic cells of the PPN as well as both LC and RN catecholaminergic neurons are active during waking, while the cholinergic cells decrease firing during SWS and the catecholamine cells groups still show activation. During REM sleep, the catecholamine cells groups are generally silent, but the cholinergic PPN cells fire in bursts, especially in the cat.
BvS-> Hypothesis: When chronic LC/NE exists (e.g. PTSD since childhood), is functioning “Normally” it rest during REM-sleep but is overactivated (too it´s chronical overactivity level) with different hard suddenly effects in a particular individual, e.g. panicing (as I of my patients, data during simulating via hypnosis show it clearly, … reference picture coming, showing also treatment effects in respiratory sinus arrythmia pattern).
After REM-sleep
Some references
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9099715/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2902103/ + https://www.naturalmedicinejournal.com/journal/2010-06/role-cortisol-sleep -> NB NB NB Rhodiola rosea is an adaptogenic herb that modulates cortisol – as well as
Interactions between sleep, stress, and metabolism: From physiological to pathological conditions https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4688585/( “However, the effects of glucocorticoids as well as CRH on REM are not well understood and most of them are contradictory [4].” “where sympathetic stress activation during dreams may not be neglected”.
